H&D Sonography, LLC
A 60 Baldwin Rd #110A, Parsippany-Troy Hills, NJ 07054
P (973) 794-1174
F (973) 866-0353
Hours of Operation
Monday – Friday: 9AM – 5PM
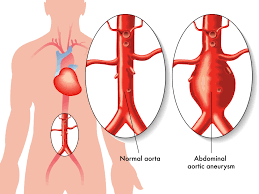
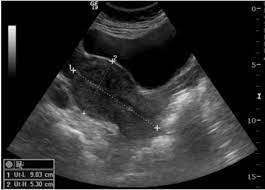
Most abdominal aortic aneurysms produce no symptoms (they are asymptomatic). They are often incidentally discovered when abdominal ultrasounds and/or CT scan studies are ordered for other conditions. When they produce symptoms, the most common symptom is pain. The pain typically has a deep quality as if it is boring into the person. It is felt most prominently in the middle of the abdomen and can radiate to the back. The pain is usually steady but may be relieved by changing position. The person may also become aware of an abnormally prominent abdominal pulsation. Abdominal aortic aneurysm can remain asymptomatic or produce mild to moderate symptoms for years. However, a rapidly expanding abdominal aneurysm can cause sudden onset of severe, steady, and worsening middle abdominal and back pain. A rapidly expanding aneurysm is also at imminent risk of rupture. Actual rupture of an abdominal aneurysm can cause sudden onset of back and abdominal pain, sometimes associated with abdominal distension, a pulsating abdominal mass and even shock (severe low blood pressure due to massive blood loss).


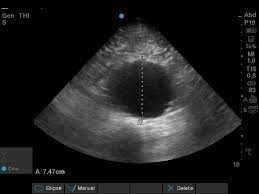
An abdominal ultrasound uses reflected sound waves to produce a picture of the organs and other structures in the upper abdomen.. An abdominal ultrasound can evaluate the: ● Abdominal aorta, which is the large blood vessel (artery) that passes down the back of the chest and abdomen. The aorta supplies blood to the lower part of the body and the legs. ● Liver, which is a large dome-shaped organ that lies under the rib cage on the right side of the abdomen. The liver produces bile (a substance that helps digest fat), stores sugars, and breaks down many of the body’s waste products. ● Gallbladder, which is a saclike organ beneath the liver. The gallbladder stores bile. When food is eaten, the gallbladder contracts, sending bile into the intestines to help in digesting food and absorbing fat-soluble vitamins. ● Spleen, which is the soft, round organ that helps fight infection and filters old red blood cells. The spleen is located to the left of the stomach, just behind the lower left ribs. ● Pancreas, which is the gland located in the upper abdomen that produces enzymes that help digest food. The digestive enzymes are then released into the intestines. The pancreas also releases insulin into the bloodstream; insulin helps the body utilize sugars for energy. ● Kidneys, which are the pair of bean-shaped organs located behind the upper abdominal cavity. The kidneys remove wastes from the blood and produce urine.
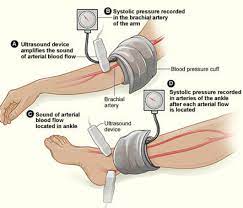
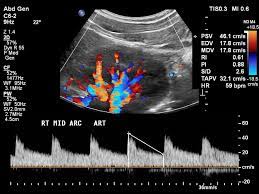
he ankle-arm pressure index (also known as the Ankle / Brachial Index or ABI) compares the systolic blood pressure of the ankle to that of the arm (brachial). These measurements are useful in the assessment, follow-up and treatment of patients with peripheral vascular disease (PVD). ABI’s provide an objective baseline to follow the progression of the disease process and evaluate the effectiveness of the treatment plan. The ABI results are usually combined with Doppler or pulse volume waveform analysis (PVR). Significant changes in arterial systolic pressure between sites indicate reduced blood flow caused by obstruction of blood vessels. The effects of obstructions can be emphasized by increasing blood flow, either by exercise testing or by inducing reactive hyperemia with an occlusive cuff. Patients, such as diabetics, with calcified vessels may show falsely elevated ankle pressures. In this case, pressure measurements can be made on the foot or toes by Photo Plethysmography (PPG) for more accurate results. Diagnostic information is obtained both from the waveform of the arterial flow when displayed on a chart recorder and from using the PPG sensor to determine the blood pressure in the digit. ABI Interpretation Levels: ● 1.3 Non-compressible ● 1.00 – 1.29 Normal ● 0.91 – 0.99 Borderline (equivocal) ● 0.41 – 0.90 Mild-to-moderate P.A.D. ● 0.00 – 0.40 Severe P.A.D.

ANS Testing: Provides quantitative assessments of the autonomic nervous system Distinguishes between early and late stages of autonomic neuropathy Recognizes up to 81 different variations in the relationship between sympathetic and parasympathetic activities. ANS testing helps you objectively confirm or exclude: ● Cardiovascular Autonomic Neuropathy (CAN) ● Diabetic Autonomic Neuropathy (DAN) ● Syncope ● Dizziness ● Distinguish between early and late stages of autonomic neuropathy ● Better monitor patient’s beta-blocker regime overdose cases ● Other dysautonomia problems A functional understanding of ANS enables you to: ● Monitor and predict general responses to a variety of stimuli ● Explain responses to changes in environmental conditions ● Manage symptoms that result from abnormal autonomic functions ● Understand how drugs affect the ANS Early detection of ANS imbalances helps broaden treatment options: ● Helps monitor patients’ overall health ● Provides early detection of Silent Ischemia ● May help prevent unexpected sudden cardiac death ● Reimbursed by most third-party payors and Medicare Early detection of ANS imbalances helps broaden treatment options: ● Diabetes ● Hypertension ● Orthostatic hypotension ● Cardiovascular Autonomic Neuropathy (CAN) ● Syncope ● Sleep apnea ● Congestive heart failure ● Chronic pain and more

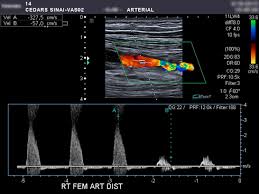
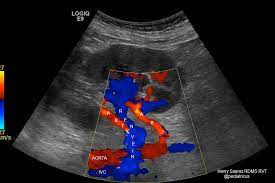
Peripheral arterial disease is estimated to affect approximately 8 – 12 million individuals in the United States. Originally, the purpose of the noninvasive arterial evaluation was to offer objectivity in the diagnosis of lower extremity arterial disease. It was intended to complement but not to replace a careful history and physical examination of the patient. Currently, after decades of evolution, the noninvasive arterial evaluation may be tailored to a patient’s specific needs, depending on the clinical presentation and the pathologic findings being evaluated. Arterial duplex imaging provides direct anatomic and physiologic information, but it does not provide information regarding overall limb hemodynamics. Duplex imaging distinguishes between a stenosis and an occlusion, determines the length of the disease segment and patency of the distal vessels, evaluates the results of intervention (angioplasty, stent placement), diagnoses aneurysms and pseudoaneurysms, and monitors a patient’s postoperative course with continuing bypass graft surveillance.

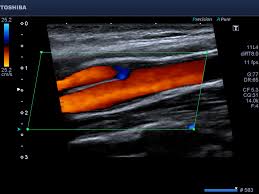
Carotid duplex imaging is now recognized as the best non-invasive screening test for carotid artery stenosis. The evidence for its use as the sole diagnostic imaging modality prior to carotid endarterectomy is examined. Providing it is carried out by experienced trained operators using validated duplex criteria, carotid duplex imaging is safe, highly sensitive and specific, and superior to angiography at plaque characterization and evaluation of flow disturbance.

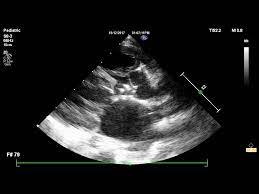
An echocardiogram, often referred as an ECHO, is an ultrasound exam of the heart. Echocardiography is used to diagnose cardiovascular diseases. IIt can provide a wealth of helpful information, including the size and shape of the heart, its pumping capacity and the location and extent of any damage to its tissues. It is especially useful for assessing diseases of the heart valves.

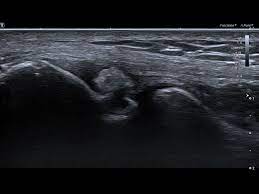
What is Ultrasound Imaging of the Musculoskeletal System? Ultrasound is safe and painless, and produces pictures of the inside of the body using sound waves. Ultrasound imaging, also called ultrasound scanning orsonography, involves the use of a small transducer (probe) and ultrasound gel placed directly on the skin. High-frequency sound waves are transmitted from the probe through the gel into the body. The transducer collects the sounds that bounce back and a computer then uses those sound waves to create an image. Ultrasound examinations do not use ionizing radiation (as used in x-rays), thus there is no radiation exposure to the patient. Because ultrasound images are captured in real-time, they can show the structure and movement of the body’s internal organs, as well as blood flowing through blood vessels. Ultrasound imaging is a noninvasive medical test that helps physicians diagnose and treat medical conditions. Ultrasound images of the musculoskeletal system provide pictures of muscles, tendons, ligaments, joints and soft tissue throughout the body. What are some common uses of the procedure? Ultrasound images are typically used to help diagnose: ● tendon tears, or tendinitis of the rotator cuff in the shoulder, Achilles tendon in the ankle and other tendons throughout the body. ● muscle tears, masses or fluid collections. ● ligament sprains or tears. ● inflammation or fluid (effusions) within the bursae and joints. ● early changes of rheumatoid arthritis. ● nerve entrapments such as carpal tunnel syndrome. ● benign and malignant soft tissue tumors. ● ganglion cysts. ● hernias. ● foreign bodies in the soft tissues (such as splinters or glass). ● dislocations of the hip in infants. ● fluid in a painful hip joint in children. ● neck muscle abnormalities in infants with torticollis (neck twisting). ● soft tissue masses (lumps/bumps) in children.
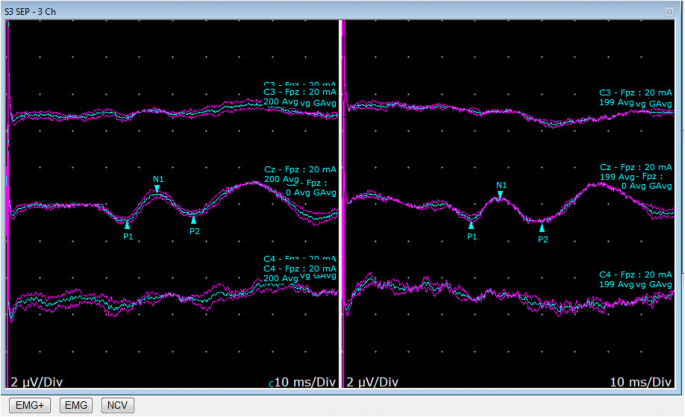
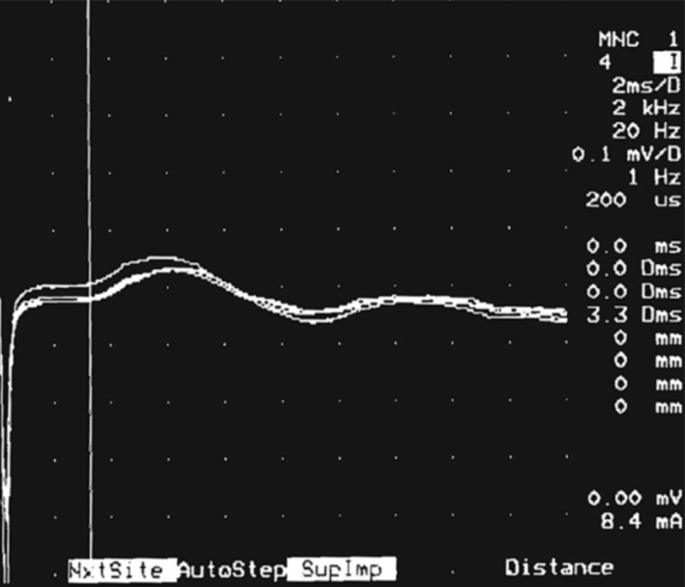
Nerve conduction velocity Nerve conduction velocity (NCV) is a test to see how fast electrical signals move through a nerve. How the Test is Performed Patches called surface electrodes are placed on the skin over nerves at various locations. Each patch gives off a very mild electrical impulse, which stimulates the nerve. The nerve’s resulting electrical activity is recorded by the other electrodes. The distance between electrodes and the time it takes for electrical impulses to travel between electrodes are used to determine the speed of the nerve signals. SSEP: Somatosensory Evoked Potential: SSEP’s assess the speed of electrical conduction across the spinal cord and are sometimes ordered for patients with back pain. If the spinal cord is significantly pinched, the electrical signals will travel slower than usual. SSEP’s may also be used to monitor spinal cord function during surgical procedures, although since the spinal cord ends before the lumbar spine, this is usually of limited value during lumbar spinal surgery and it is used more often in cervical (neck) or thoracic (chest) spine surgery. Sympathetic Skin Repsonse (SSR): Sympathetic skin response (SSR), defined as the momentary change of the electrical potential of the skin, may be spontaneous or reflexively evoked by a variety of internal or by externally applied arousal stimuli. Although the suprasegmental structures influencing the SSR in humans are not well known, SSR has been proposed as a non-invasive approach to investigate the function of the sympathetic system. SSR is easy to apply but current procedures are not sufficiently reliable for diagnostic purposes, and show imperfect correlations both with clinical features and other measurements of autonomic, in particular, sudomotor dysfunction.

A pelvic ultrasound is a noninvasive diagnostic exam that produces images that are used to assess organs and structures within the female pelvis. A pelvic ultrasound allows quick visualization of the female pelvic organs and structures including the uterus, cervix, vagina, fallopian tubes and ovaries. Pelvic ultrasound may be performed using one or both of 2 methods: ● Transabdominal (through the abdomen). A transducer is placed on the abdomen using the conductive gel ● Transvaginal (through the vagina). A long, thin transducer is covered with the conducting gel and a plastic/latex sheath and is inserted into the vagina
A renal ultrasound is a safe and painless test that uses sound waves to make images of the kidneys, ureters, and bladder. The kidneys are a pair of bean-shaped organs located toward the back of the abdominal cavity, just above the waist. They remove waste products from the blood and produce urine. The ureters are thin tubes that carry the urine from the kidneys to the bladder. During the examination, an ultrasound machine sends sound waves into the kidney area and images are recorded on a computer. The black-and-white images show the internal structure of the kidneys and related organs.

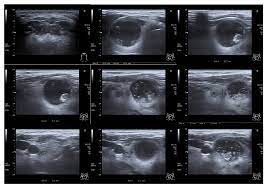
An ultrasound of the thyroid produces a picture of the thyroid gland. The thyroid gland is located in front of the neck just below the Adam’s apple and is shaped like a butterfly, with two lobes on either side of the neck connected by a narrow band of tissue. It is one of nine endocrine glands located throughout the body that make and send hormones into the bloodstream. An ultrasound of the thyroid is typically used to help diagnose: ● a lump in the thyroid ● a thyroid that is not functioning properly Because ultrasound provides real-time images, it also can be used to guide procedures such as needle biopsies, in which needles are used to extract sample cells from an abnormal area for laboratory testing. Ultrasound may also be used to guide the insertion of a catheter or drainage device and helps assure accurate placement.

Loop Memory Cardiac Event Recorder ● Recessed RECORD BUTTON prevents accidental patient activations; ● Memory Capacity Up To 21 Minutes; ● Powered by 1AA Alkaline battery (w/ 30 day battery life); ● Eight Program Options offer variety of Pre and Post recording times; ● Clearly marked SEND BUTTON and a RESET BUTTON that will only clear the device’s memory after the patient has sent stored ECG’s.

We use Videonystagmography (VNG) technologies for testing inner ear and central motor functions. VNG testing is considered the new standard for testing inner ear functions over Electronystagmography (ENG), because VNG measures the movements of the eyes directly through infrared cameras, instead of measuring the mastoid muscles around the eyes with electrodes like the previous ENG version. VNG testing is more accurate, more consistent, and more comfortable for the patient. By having the patient more comfortable and relaxed, consistent and accurate test results are more easily achieved. VNG testing is used to determine if a vestibular (inner ear) disease may be causing a balance or dizziness problem, and is one of the only tests available today that can decipher between a unilateral (one ear) and bilateral (both ears) vestibular loss. VNG testing is a series of tests designed to document a persons ability to follow visual objects with their eyes and how well the eyes respond to information from the vestibular system. This test also addresses the functionality of each ear and if a vestibular deficit may be the cause of a dizziness or balance problem. To monitor the movements of the eyes, infrared goggles are placed around the eyes to record eye movements during testing. VNG testing is non-invasive, and only minor discomfort is felt by the patients during testing as a result of wearing goggles. Appointments usually last about 1.5 hours, and testing is covered by all insurances. There are 4 main parts to a VNG test: 1. Occular Mobility You will be asked to have your eyes follow objects that jump from place to place, stand still, or move smoothly. The technician will be looking for any slowness or inaccuracies in your ability to follow visual targets. This may indicate a central or neurological problem, or possibly a problem in the pathway connecting the vestibular system to the brain. 2. Optokinetic Nystagmus You will be asked to view a large, continuously moving visual image to see if your eyes can appropriately track these movements. Like the occular mobility tests, the technician will be looking for any slowness or inaccuracies in your ability to follow visual targets. This may indicate a central or neurological problem, or possibly a problem in the pathway connecting the vestibular system to the brain. 3. Positional Nystagmus The technician will move your head and body into various positions to make sure that there are no inappropriate eye movements (nystagmus), when your head is in different positions. This test is looking at your inner ear system and the condition of the endolymph fluid in your semi-circular canals. The technician is verifying that small calcium carbonate particles called otoconia are not suspended in the fluid and causing a disturbance to the flow of the fluid. 4. Caloric Testing The technician will stimulate both of your inner ears (one at a time) with warm and then cold air. They will be monitoring the movements of your eyes using goggles to make sure that both of your ears can sense this stimulation. This test will confirm that your vestibular system for each ear is working and responding to stimulation. This test in the only test available that can decipher between a unilateral and bilateral loss.
A 60 Baldwin Rd #110A, Parsippany-Troy Hills, NJ 07054
P (973) 794-1174
F (973) 866-0353
Monday – Friday: 9AM – 5PM